
Figure 1 A Fischer diathermy machine, circa 1920.
The benefits of electromagnetic energy for treating medical conditions have been recognized since the late 19th century. Today, although probably only magnetic residence imaging (MRI) is familiar to most people, many other medical applications exploit its unique abilities. They include reducing the size of tumors, aiding cardiac surgery, rejuvenating skin and treating muscular conditions. Medical systems based on RF energy are continually advancing, thanks in large measure to the transition from vacuum tubes to solid-state. Semiconductor devices such as LDMOS bring flexibility, enable advanced modes of operation and offer advantages at microwave frequencies.
SPARK OF INSPIRATION
The benefits of RF energy in almost all medical applications are gained from heat generated by some form of RF generator. Although the first recorded evidence of heat from any source used for medical purposes dates to prehistoric times, when heated rocks were used to reduce or stop blood flow (hemostasis), it was the prodigious inventor and scientist Nicola Tesla who first proposed, in 1891, that the application of electricity could produce heat in a human body. This was dangerous territory, as electricity caused electric shock. Shortly after Tesla’s results were presented, French physician and biophysicist Jacques Arsene d’Arsonval discovered that when the frequency of this energy was above 10 kHz, rather than shocking the patient, it caused the skin to heat. He proposed ways of applying this “high frequency” current to the body using contact electrodes, capacitive plates and inductive coils.
The use of RF energy to heat deep tissue was first suggested by Austrian chemist R. von Zaynek, who noted that production of heat in tissue was a function of both frequency and current density. In 1908, German physicist Karl Franz Nagelschmidt coined the name “diathermy” for this, during what were the first extensive experiments on humans. Nagelschmidt is considered to be the pioneer in the field, writing the first textbook on the subject in 1913. Important developments in later years included those of Harvey Cushing and William T. Bovie, in which an electrosurgical device developed by Bovie was used to cause homeostasis during the resection of a vascular brain tumor.
The initial use of RF energy for diathermy was impeded by the lack of devices to generate it, as spark-discharge Tesla coil machines could reach frequencies of only 2 MHz. This type of diathermy was called longwave diathermy, because of the long wavelengths at these frequencies. The invention that broke this logjam was the vacuum tube, revealed in 1904 by John Ambrose Fleming, which ultimately increased the frequency to about 300 MHz (see Figure 1). Diathermy machines operating at this frequency were called shortwave diathermy. Like many RF and microwave technologies, the advancement of vacuum tube technology dramatically accelerated during the world wars, and new types of vacuum electron devices were created. The most noteworthy was the magnetron, which made it possible for emerging radar systems to generate high power at higher frequencies. One of the beneficiaries of the magnetron has been the medical profession, and many of the initial applications are still in use today and still use magnetrons for generating RF energy.
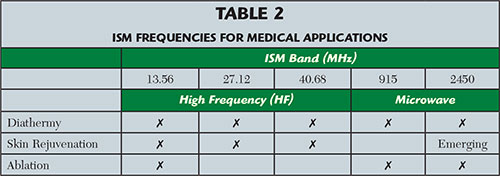

Figure 2 Microwave diathermy treatment.
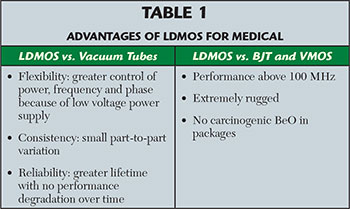
Like vacuum tubes before them, transistors further extended the reach of RF energy medicine. The earliest examples of transistor-based power generation appeared in the 1950s, although these devices generated minimal power and were extremely fragile. As their limitations were mitigated in subsequent years, semiconductor technologies such as the bipolar junction transistor (BJT) and vertical metal oxide semiconductor (VMOS) transistor were adopted for medical devices. Today, laterally-diffused metal oxide semiconductor (LDMOS) power transistors are proving to be the preferred solid-state technology, producing power levels up to 1500 W. LDMOS transistors have advantages that make them well suited to be the alternative to their vacuum tube and transistor predecessors (see Table 1).
The primary benefit transistors have over vacuum tubes for medical applications is flexibility. The output power can be tightly controlled over their full dynamic range, which enables heat transferred to human tissues to be reduced when required. They support sweeping frequencies within an ISM band (from 902 to 928 MHz, for example), which helps to maximize the energy transferred to the body. For advanced systems that use multiple probes to combine wave fronts, the phase can be controlled to move the areas that must be targeted. While vacuum tubes require potentially dangerous high voltages, generated by large and heavy power supplies, transistors operate at 32 to 50 VDC. The biggest advantages of LDMOS transistors over previous semiconductor technologies are their ability to operate at higher frequency, such as 915 and 2450 MHz, and ruggedness. LDMOS power transistors will survive when almost all the transmitted energy is reflected back, because of an impedance mismatch such as a short or open circuit. This is important in medical applications because human tissue can present a variable load to the probe.
Originally, the capabilities of available RF power sources determined the frequencies where electromagnetic energy-based systems were used. The first operating frequencies were very low, with both frequency and output power increasing over time. However, as medical, scientific and industrial systems began to proliferate, it became necessary to specify areas of the electromagnetic spectrum for operation. These industrial, scientific and medical (ISM) bands for the U.S. are shown in Table 2, and are widely accepted throughout the world. Some countries use additional frequencies. Many other systems operate in these same bands, including Wi-Fi, Bluetooth, microwave ovens and RF-based industrial equipment. With ISM bands unregulated, equipment must prevent or tolerate interference generated by nearby applications.
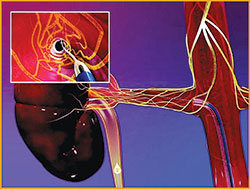
Figure 3 Microwave ablation used for renal denervation.
RF HEATING OF TISSUE
With the exception of MRI— which uses an intense electromagnetic field for imaging, not heating—all medical applications use RF to create heat. The electromagnetic field applied at high frequencies forces the water dipole to move with every cycle, creating friction between the molecules and generating heat. The frequencies at which this heat is generated and the hardware used to apply the heat largely determine the utility for specific medical uses. Generalizing about the use of electromagnetic energy for medical applications:
- Changes in tissue occurring at the molecular level differ with frequency
- Lower frequencies penetrate deeper into the skin than higher frequencies
- Lower frequencies penetrate fewer types of tissue than microwave frequencies
- Systems operating at microwave frequencies can more precisely direct energy to specific areas
- Medical systems operating at lower frequencies have been in use far longer than microwave-based systems that operate above 900 MHz
- The advantages of systems operating at microwave frequencies are gaining importance and becoming more thoroughly understood.
After the early efforts by Tesla and others suggested an interaction between radiated electromagnetic energy and the human body, the mechanism was further clarified and extended to all non-conducting materials. It was shown that the depth of penetration is determined by the frequency of the radiation and the insulating properties of the material. When microwave generators became available, it was demonstrated that because of their short wavelengths, specific areas could be targeted precisely. Greater penetration at lower frequencies (to about 2 inches) makes lower frequencies desirable for applications such as diathermy, in which the goal is often to soothe aching muscles. Microwave frequencies offer benefits such as faster heat delivery, more precise targeting of specific areas (a tumor, for example) and more accurate control.
At low frequencies, the electromagnetic field is generated between two or more electrodes, the shape dictating the characteristics of the field. The most common types of electrodes are rods and plates, between which the target material is placed. With increasing electrode distance, the voltage to maintain the electric field strength also increases, and the maximum distance between the electrodes and, thus, the maximum thickness of the target material is determined. When microwave frequencies are used, the energy is launched from a small emitter and guided through space to the target; a set of plates, used with lower frequency applications, is not required.
Arguably, there are dozens of medical applications that use RF energy, either alone or in combination with light or a laser at various wavelengths. However, they generally fall into the following categories: MRI, diathermy, ablation and skin rejuvenation. MRI will not be discussed, because its benefits are not derived from heat.
DIATHERMY
As the first treatment to use electromagnetic energy, diathermy has a long-established track record of effectiveness, and its use has expanded dramatically over the years. Today, diathermy either applies heat directly to the skin (shortwave diathermy) or heats it using a probe situated a short distance from the body that directs energy to the skin (microwave diathermy). Shortwave diathermy operates at 13, 27 or 40 MHz, and microwave diathermy operates at either 915 or 2450 MHz. Although vacuum tubes have long been used as the RF power source for both shortwave and microwave diathermy, LDMOS power transistors are replacing them, due to their longevity; precise control of power level, frequency and phase; simpler control mechanisms; smaller amplifier size and lower operating voltage (see Table 1).
Shortwave diathermy employs either two plates, placed on either side of the area of the body to be treated, or induction coils, molded to fit the body or wrapped around a limb. As the high frequency waves travel through the body tissues between the plates or coils, they generate heat. The degree of heat and depth of penetration partially depend on the absorptive and resistance properties of the tissues that the waves encounter. Shortwave diathermy is most effective for treating pain caused by sinusitis, kidney stones and pelvic infections, as well as conditions that cause muscle spasms.

Figure 4 Before (a) and after (b) skin rejuvenation using RF energy.
Microwave diathermy is very effective for evenly warming tissues without heating the skin. Unlike shortwave diathermy, microwave diathermy does not apply heat directly to the body, rather beams RF energy into it from a probe to generate heat within the targeted tissues (see Figure 2). As it cannot penetrate deep into muscles, the primary applications are for areas closer to the skin, such as shoulders. The probe focuses the RF energy field directly on the targeted tissue in a more concentrated area than shortwave diathermy. Absorption of the energy causes heating in the tissues, deeper than infrared treatments but not as deep as shortwave diathermy.
As heat increases, so does blood flow, which can improve flexibility in joints and connective tissue. As pain and inflammation are reduced, arthritis sufferers can increase the range of motion. Other applications include treatment of sprains, strains, lesions, degenerative joint disease, rheumatoid arthritis, stiffness in the joints, hematoma, bursitis, synovitis, infected surgical incisions, carbuncles and abscesses. Diathermy can be used for surgical procedures, where a probe is applied to a blood vessel to cause the blood to coagulate, cauterizing the area. It is also effective in removing tumors in cases where traditional surgical techniques are impractical, such as the prostate, bladder, cervix, brain, ovaries, bowels and tonsils.
ABLATION
Ablation, in medical terms, applies to any technique (including surgery) that destroys tissue for a specific beneficial purpose. Two types of ablation systems use RF energy: RF ablation typically operates between 450 and 500 kHz and microwave ablation operates at either 915 or 2450 MHz. RF and microwave ablation are principally employed for heart surgery and tumor reduction and removal. Increasingly, they are considered a first-line treatment. RF ablation is the most widely used technique, while microwave ablation treatment is growing as studies show where its operating frequency provides unique benefits. The ablation procedure is typically guided by images generated by MRI, computed tomography (CT) or ultrasound, enabling the surgeon to precisely address a specific location with the ablation electrode. The electric current produced by the RF power source causes tissue heating around the probe at temperatures high enough to cause tissue death.
There are two types of RF ablation: monopolar and bipolar. In monopolar RF ablation, a single group of electrodes delivers energy at the tumor site using a ground pad to complete the circuit through the body. The pad, which acts as a return path for the RF current, is generally located on the patient’s thighs or back. Bipolar RF ablation allows current to flow between multiple groups of electrodes and does not require the use of grounding pads. The procedure is performed by inserting the probe into the target tissue to be destroyed. Tissue is heated by applying current between the probe and the ground pad or other electrodes. To ensure that tissue heating occurs only where desired, some parts of the probe may be insulated. Cell death depends on temperature and application time, ranging from a few minutes to kill cells at 50°C and just a few seconds at higher temperatures.
In many cases, microwave ablation has advantages over its low frequency counterpart. Molecules continuously realign as the microwave energy field oscillates, which increases kinetic energy and tissue temperature. Because of its small wavelength, the amount of energy delivered around the probe is denser and makes the procedure faster. Unlike lower frequency currents, energy at microwave frequencies can permeate all biological tissues, including bone and lungs that resist electric current. Consequently, microwave ablation generates a greater volume of energy around the probe, expanding the ablation zone and potentially reducing the number of required applications. The design of the microwave probe is a major determinant of the shape and size of the ablation zone. Researchers have produced many types of probes with varying degrees of effectiveness at controlling the transfer of RF energy. More than one probe can be used to create a larger ablation zone that precisely conforms to the target area. The phase of the signal at each probe can be varied to create zones of constructive and destructive wave interaction, yielding a positive effect on the results.
The benefits of microwave ablation versus RF include reduced application time (as little as a few minutes), higher temperatures, reduced sensitivity to various types of tissue, reduced need to reposition the probe and the ability to treat tumor types where RF ablation cannot be used.
Another use of ablation is renal denervation (see Figure 3), the subject of research for its potential to treat hypertension in patients for whom medication and other traditional remedies are not effective. It is a minimally-invasive procedure that reduces blood pressure by ablating the renal nerves. A small catheter is placed in the femoral artery, which provides access to the nerves serving the renal artery. The nerves are ablated by passing electromagnetic energy into the artery through the catheter tip placed in the kidneys. The energy is transmitted through the vessel wall to damage the renal nerves.
SKIN REJUVENATION
Many techniques that fall within the broad term of cosmetic therapy (also called esthetic therapy) employ RF energy, either alone or in combination with a laser or other source of light (see Figure 4). Optical energy has been used for many years for treating dermatologic problems, sometimes combining lasers and intense pulse light (IPL) for epilation, removal of vascular and pigmented lesions, reduction of fine wrinkles and acne treatment. In most cases, the laser’s power is generated by an RF source; power levels of several kilowatts at a frequency of 100 MHz create a plasma in a chamber, from which the laser light is extracted.
The limitations of optical techniques caused researchers to investigate the use of RF energy, which has become very popular. RF treatments rely on the tissue’s electrical properties rather than on the concentration of molecules in the skin for thermal destruction. RF technology transfers energy to the skin at relatively low temperatures, so it is well suited for acting on dermal collagen without affecting the epidermis, which enables more effective wound healing and provides effective skin rejuvenation in a short time (see Figure 5). As it does not affect epidermal melanin, patients of all skin types can be treated, including those with darker skin and those prone to developing post-inflammatory hyperpigmentation.
Figure 5 Cross section of human skin. Source: Henry Gray, “Anatomy of the Human Body,” 1918.
There are several approaches to RF-based treatments: Monopolar RF applies a single electrode tip to the target area, and another plate serves as a ground pad. Bipolar RF targets tissue using two points on the tip of a single probe, and tripolar RF employs multiple electrodes to heat both shallow and deep layers of the skin at the same time. A relatively new technique, called fractional RF, uses a very thin, needle-type electrode that can service multiple zones of tissue without affecting the epidermis and adnexa, which results in faster healing. Another approach, called unipolar RF, works without delivering current to the skin. Rather, it uses energy to induce rotational oscillations in water molecules, targeting the reticular dermis and subcutaneous junction, in contrast to the bipolar technique that affects the papillary and mid-level dermis.
One skin rejuvenation application can reduce or eliminate telangiectasia (commonly called varicose veins), a skin condition that can be benign or a symptom of underlying and sometimes serious illness. Often referred to as spider veins owing to its web-like appearance, it is recognized by tiny blood vessels that cause a threadlike appearance on the skin and can form in clusters. Studies show that RF and possibly microwave ablation can reduce the plaques typical of this disease, using lower temperatures and with fewer side effects. The technique called VNUS Closure, introduced by VNUS Medical Technologies in 1998, is a similar approach that uses an injected saline solution to numb the leg, squeeze blood from the vein and protect surrounding tissue. After the procedure, blood is naturally rerouted through other healthier veins.
A cosmetic procedure called body contouring allows reshaping of the body without surgery and has resulted in numerous noninvasive and often proprietary techniques. RF energy is used to deliver current deep into areas of fat cells to destroy them. Connective tissue and fat both contribute to the development of cellulite, for which RF energy has proven to be effective in minimizing. The heat produced causes collagen proteins in connective tissue to change and tighten. Studies have shown that it may also increase blood flow and fat metabolism at the treatment site. RF energy also affords its noninvasive capabilities for liposuction. Radio frequency assisted liposuction (RFAL), a technique developed by one manufacturer, uses RF energy to produce heat using two electrodes, one external and one internal and connected to a handheld controller.
Electro-optical synergy (ELOS), also called E-light technology, combines bipolar RF and optical energy to reduce the intensity and potential side effects of optical energy. Studies have shown that it can be used with all hair types and is effective in removing white hair.
EMERGING APPLICATIONS
RF technology is being used to treat other pathologies, and many rely on RF ablation. It is being used to treat various heart conduction disorders, of which there are many. The procedure has been demonstrated to be safe, with a mortality rate of less than one per 2,000 procedures. RF ablation is also being used to treat hepatocellular carcinoma, the most common type of liver cancer. Electrodes are inserted into the liver tumor using percutaneous, laparoscopic or open surgery with guidance from ultrasound imaging. As it is a local treatment with minimal effects on normal healthy tissue, it can be repeated multiple times. The technique has proven to have four-year survival rates like those of surgical resection. Barrett’s esophagus, a serious complication of gastroesophageal reflux disease, is also being treated using RF ablation. The RF energy is delivered through an endoscope inserted into the esophagus that allows abnormal cells to be destroyed while protecting the healthy cells underneath.
Conclusion
The use of RF energy in medicine has a long history and has proven its effectiveness, either alone or used with a laser for diathermy, ablation and skin treatment. Advances in solid-state device technology enable better control and flexibility, especially LDMOS RF power transistors that extend treatment options to microwave frequencies.
